“Not everything that is faced can be changed,
but nothing can be changed until faced.”
-James Baldwin
FROM THE BATTLEFIELDS TO HOSPITALS HALLS AND TO OUR HOMES, WE HAVE GOT TO CONTINUE
TO FIGHT AGAINST THE INVISIBLE ONES.
Nurse Nightingale work in the Crimea still supports good hand hygiene reduces infections. As the administrator of the army hospital and her band of nurses at Scutari, Nightingale made critical observations. She saw severely wounded soldiers carried directly from the battlefield into the operation room by the same medics who would perform their amputations. There was no provision for scrubbing before a case or even hand washing between cases. The rate of post operative infections soared. She continued to keep a watchful eye not only on operative cases but in the day-to-day treatment of injured soldiers. Once Florence found the number one factor which contributed to the rapid spread of infection, she made up her mind to do something about it.
Here we are one hundred and sixty-nine years later nurses are still struggling with this evidenced based practice. “ Come, let us reason together!” An admonition from the ancient prophet Isaiah to a select group of people. Nurses are the crème de la crème of the health care profession. They are a singled out and set apart group of frontline workers.
THE NURSES ROLE
Nurses work closely with doctors and the health care team. Doctors know personally know the impact of infections on postoperative healing. Nurses know how easy it is for patients they encounter to contract common hospital infections as they go from room to room. Handwashing is imperative. Nurses also have the responsibility of educating patients, visitors, and their families about the importance of proper hand hygiene among other things.
Hospital administrators know the monetary impact of prolonged hospital stays. In 2009, Medicare, a major player in US healthcare, stopped reimbursing hospitals for what they concluded were “preventable diseases” which included hospital acquired infections from ventilator associated pneumonias (VAP) to catheter associated urinary infections (CAUTI). According to a meta-analysis conducted by the Agency for Health Care Research and Quality, the average cost per patient for prolonged hospital stay is $31, 000 compared to the average $25,000 for an uneventful stay . The monetary impact relating to prolong hospital stay forced hospitals to do something about reducing hospital acquired infections. The increasing rates of infection and mortality rates soon carved out a niche for its own specialty, Infectious disease doctors and nurses.
HAND WASHING IS STILL THE NURSE’S MOST LETHAL WEAPON AGAINST INFECTION
Infectious disease (ID) doctors help identify and treat infections including hospital acquired infections. These nurses receive additional training to help identify and treat infections. These nurses are on specialized groups like the Intravenous (IV) Team who are responsible to place, change, and remove central venous lines using strict sterile technique. Studies show that central venous lines are linked to high mortality rates caused from infections entering the blood stream. These infectious disease nurses ensure all staff are wearing the proper Personal Protective Equipment (PPE) before encountering blood and body fluids of an infectious patient and engaging in proper hand hygiene. These nurses, like Nightingale are doing something to reduce infection rates in hospitals. With all of this in place nurses are still struggling with the practice of good handwashing.
Back in the Crimea, Nightingale was taking serious notations about the increasing loss of lives amongst wounded soldiers and post-surgical amputations. She would use her findings as leverage to demand supplies from the Secretary of War at home in England to improve conditions in Scutari. Florence observation became a longitudinal study from the time of her arrival in Scutari in 1853 to the end of the Crimean war in March 1856. Nightingale’s work would later become the sounding board for evidence-based practice in modern nursing.
EVIDENCED BASE SURVEY
A joint survey of 772 health care workers conducted between NursingNote and Nursem indicated that things have worsened for nurses since the pandemic. Before the pandemic nurses washed their hands 48 times /day. During the pandemic handwashing increased to eighty-one times/day. They were compliant with fighting infections, but they notice skin changes. Health care workers noticed their hands were cracking , peeling, and becoming painful because they did not have access to hand care products such as a moisturizing lotion. Ahhh! So, there you have it! Nurses are experiencing occupational dermatitis and other skin conditions with more frequent hand washing.
THREE PLACES WHERE HAND WASHING MATTERS MOST
- In our workplaces: Wash your hands before and after work, using restrooms, eating your meals, performing procedures, administering medications, and patient contact.
- In our homes: Make washing your hands a priority on arriving home. Before starting meal preparations. Nurses are excellent teachers. Educating patients about their diseases, medications, and procedures make them good at it. Teaching others in the home proper hand hygiene is easy to do at home. What better way to remind the kids especially that, “we are all in this together.”
- When we visit other people’s homes: Families, friends, and patients. Home health and visiting nurses are good at this.
I spoke with my old friend Lisa, a home health nurse in one of the busiest cities, NEW YORK CITY. I asked her how she is coping with frequent handwashing in her line of work. She shared these two scenarios with me to demonstrate her need for flexibility is based on what her patients have available.
“ I have senior patients I see three times weekly for post operative dressing changes. They are from two different socio-economic status. One lives on Park Avenue in a beautiful penthouse. My other patient is Hispanic and speaks fluent English. Her husband worked hard but no one told him about contributing to social security. His pension would have been helpful to her now. The heating system is extremely poor in her building but finds a way to keep warm. Both women are widowed and lives alone.
“ I usually visit Ms. Park Avenue first; she has no family, but she does have a full-time housekeeper and friends at her disposal.” The door man is hilarious. “Come on in Nurse Malcom” Frank always greets me with one hand behind his uniformed back, looking as feathered as Marcus Garvey in his hay days.
“Hi Frank, is it cold enough for you today?” I glided through the door and on to the elevator like royalty.
“Thanks to this uniform my dear, and this expensive pair of leather gloves, I can’t say I feel a tinge of cold.” He always his reply. He takes my nursing bag, announces my arrival to my patient then escorts me up. Frank keeps me in stiches all the way to her penthouse where the elevator opened directly into her foyer. The first room off the foyer is a guess bathroom where I was my hands and dry them. Frank places the bag on a beautiful granite table she placed there just for the nurses and therapists who comes to see her in-home. The helper takes my coat and prepares tea while I do the dressing changes.
“ I accept a hot cup of tea from her in winter because her place is clean and well-kept. This is how we developed a trusting relationship. For the most part, I can maintain good hand hygiene because she has the facilities. Some homes don’t have even half of that!”
My other patient is an example of limited resources. One hour later, I am heading to my second patient’s home. She lives in Spanish Harlem, in El Barrio, at 96 and 5th Avenue. I don’t ride the elevators as a rule, I feel hemmed in if anyone else comes in. In these buildings I take the stairs with my mask on and my pepper spray in my hand. I need the exercise anyway, she laughs.
This apartment is clean, but the ventilation is very poor and there is little anyone can do about it. This is all she can afford. The bathroom is moldy because there is no light coming in and she hardly turns on the light because she is afraid it will run up the electric bill even more that she already is. So, I head towards the only other place in her home to wash my hands – the kitchen sink.
“I am still waiting for my disability to come through” pointing toward her oven door propped open with a long kitchen knife.
“I called the Social Security office to check on it for you yesterday and they are working on it. They will send you a letter in the mail to be see their doctor before they can approve you” I reassure her.
In a situation like this I spread newspaper on the kitchen counter before placing my bag as a barrier to reduce contact with anything infectious. Then I do my dressing changes, spend a little extra time with her and I am out. Nurses must stay flexible.
What never ceases to amaze me, Lisa concludes, is the difference between these two human beings who only live twenty blocks apart from each other. When I cut through Central Park is only ten blocks or so. But one is so much more susceptible to injury and infection than the other. One has more access to health care. Regardless of their situation, my is to keep them both from going back to the hospital because of an infection. To do that, I make sure I maintain proper hand hygiene.
Florence Nightingale could not change the fact that over 130,000 British soldiers died from infectious diseases in the Crimean War. Instead, she faced Dr. Barry’s wrath and challenged the Secretary of War, to do something to improve sanitation and overcrowding. In 1855 a group of sanitation officials arrived in Scutari and under the leadership of Nurse Nightingale, they assessed the conditions and made the necessary improvements. The mortality rate plummet from 41 percent to 2 percent by the end of the war according to Science Museum UK.
WE ARE ALL NIGHTINGALES
Nurses, you cannot change the past, but you must challenge the future. Florence Nightingale’s observation became a longitudinal study from the time of her arrival in Scutari in 1853 to the end of the Crimean war in March 1856. Her work would later become the sounding board for evidence-based practice in modern nursing. Nurses you are gamechangers. Wherever you are employed in the profession of nursing you can model this behavior. Proper handwashing still saves lives.
Handwashing will continue to help battle the pandemic. We still see viruses emerging silently like Omicron and Monkey Pox. As the health care team head into the Fall of 2022, nurses carry around the antidote to these infectious diseases. It is the most lethal weapon, and it is also the least expensive. Good Handwashing.
A NURSE TO THE RESCUE
A pediatric cardiothoracic nurse, Antonia Philp, who was also experiencing dryness and skin irritations due to frequent hand washing came up with a brilliant solution. She now sells a brand of hand moisturizing hand cream branded as Nursem.
We Care About Nurses support Nursem, in doing so we promote good hand washing and excellent hand care. When you support Nursem, Antonia will give a nurse a free hand lotion with your purchase. Help one nurse at a time prevent occupational dermatitis with each purchase.
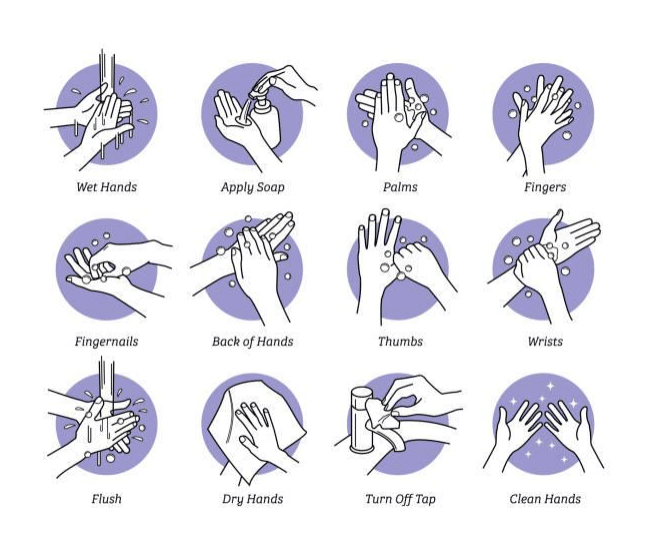
Hand washing technique reminder